Atrial septal defect (ASD) is a hole in the muscular wall (interatrial septum) between the two upper chambers of the heart (atrium). Such deficiency leads to communication between both atria, which, if sufficiently large, can lead to a reversal of blood flow and consequently to many disorders such as heart failure, pulmonary hypertension, stroke, heart rhythm disturbances.
It is one of the most common congenital heart defects. There are many forms of defect, but the most common is the so-called type secundum, in which the described communication is located at the very middle of the septum.
Diagnosis is often made during adulthood because patients have no symptoms or have minimal symptoms.
For the last several decades, the treatment has been purely surgical, but today the method of percutaneous defect closure is being used with the help of so-called occluder, which is also available at our institution since 2018.
Procedure
Prior to the procedure, each patient is fully explained the benefits and potential risks of the procedure (informed consent of the patient). It should be noted that before and after the procedure, it is mandatory to take dual anti-aggregation therapy (acetylsalicylic acid plus clopidogrel) for a minimum of 3 months, due to the risk of thrombosis of the device. Prophylaxis of bacterial endocarditis is also required up to 6 months after surgery.
As part of the preparation for the procedure, a transesophageal ultrasound (TEE) is performed to determine in more detail the characteristics of the septal defect itself for better planning of the intervention (type of defect, size, anatomic borders). The same method excludes the existence of a thrombus in the left atrial appendage.
The procedure is performed by introducing a catheter via the groin vein, with previous local anesthesia of the injection site and intravenous titration of the analgosedation. The catheter is then placed first through the vein into the right atrium and then through the atrial septal defect into the left atrium. An ultrasound probe (TEE) is also placed in the esophagus during the procedure, through which the optimum position of the occluder can be clearly visualized, as well as early complications of procedure (alternatively, an intracardiac ultrasound can be placed via another groin vein).
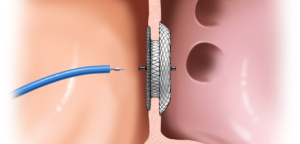
When the sheath is positioned in an adequate anatomic location, the occluder is slowly released until it ‘sits’ on the septum defect. The septal occluder use din our center consists of two disks composed of nitinol and polyester, which are interconnected by a short central part that completely fills the defect. The very composition of the occluder enhances the process of closing the defect in such a way that in the weeks after the procedure it stimulates the device to grow into cardiac tissue, which definitely closes the defect.
The success rate of the procedure is extremely high (98% successfully closed ASD 12 months after the procedure) with a low risk of complications (<1%).
The day after the procedure, a control transthoracic ultrasound of the heart is performed, and it should be repeated within the control monitoring 3 months after the procedure.
The patient is most often discharged home day after the procedure if the postprocedural course is uneventful.