Electrical cardioversion, often called (electro)cardioversion, is a procedure that treats abnormal and usually fast heart rhythm (cardiac arrhythmia). The most commonly treated arrhythmia with cardioversion is atrial fibrillation. Other cardiac arrhythmia which are treated in the same way are some circular supraventricular arrhythmias, such as atrial flutter, and ventricular tachycardia. During electrocardioversion under controlled environment, an electrical “shock” is delivered through the chest to restore normal heart rhythm.
How does electrical cardioversion work? Cardioversion includes the delivery of electrical shock across the patient’s chest to the heart muscle in order to interrupt the circulation of the tachycardia and allow the normal physiological (sinus) rhythm of the heart to be awaken.
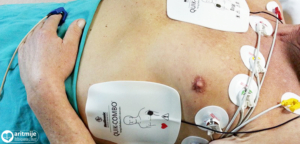
How is electrical cardioversion performed? Electrical cardioversion is performed in a specially equipped room (intensive care unit, ward, EP laboratory) where patient’s heart rate, blood pressure, respiration and blood oxygen level (saturation) is monitored. In order to make delivery of electric shock less painful for the patient, the procedure is performed under short-term general anaesthesia. In that way the patient does not feel the electric shock, nor does he/she remember the procedure. After the patient has been sedated/anaesthesized, two electrodes are positioned on the chest which has been shaved beforehand. One electrode is positioned on the right side of the sternum and the other electrode is positioned on the left side of the chest, approximately above the heart. A controlled electroshock between the two electrodes is then delivered to interrupt the abnormal heart rhythm. The energy level is determined by the doctor depending on the arrhythmia, and if the first attempt is unsuccessful, the shock can be repeated with higher energy levels. After the patient is sedated/anaesthesized, the electrical cardioversion itself takes a few seconds, and the time required for the patient to wake up is approximately 5 to 10 minutes.
Electrical cardioversion in patients with an implanted cardiac pacemaker or implantable cardioverter defibrillator (ICD). With patients who have an implanted cardiac pacemaker or an ICD some caution is needed. Cardioversion can disrupt the pacemaker’s or ICD’s function, may damage the pacemaker’s casing, electrodes, or heart tissue. In order to reduce the risk, the external defibrillator electrodes should be placed at least 12 cm from the implanted device or, most commonly, the electrodes should be placed in the middle of the thorax and on the back between the shoulder blades (the anteroposterior position). Before and after electrical cardioversion, the implantation device requires testing in order to ensure that it is working properly.
Treatment after electrical cardioversion. After cardioversion, the patient is monitored for several hours, and if no additional medical treatment (hospitalization) is planned, he or she can be discharged. Recommendation is that the patient is discharged in company of a relative or a friend. A patient who was under sedation during cardioversion should not drive vehicles for 24 hours due to the possible side-effects of anaesthesia. Some patients may have skin irritation in the area where cardioversion electrodes were attached and recommendation is that the skin is treated with soothing creams to reduce irritation.
Electrical cardioversion in pregnancy. Cardioversion can be performed during pregnancy without affecting the fetal heart rate. However, recommendation is to monitor the fetal heart rate during the procedure.